
What is Parkinson's Disease? What Medical Assistive Devices Do they Need?
2024-09-02 15:30
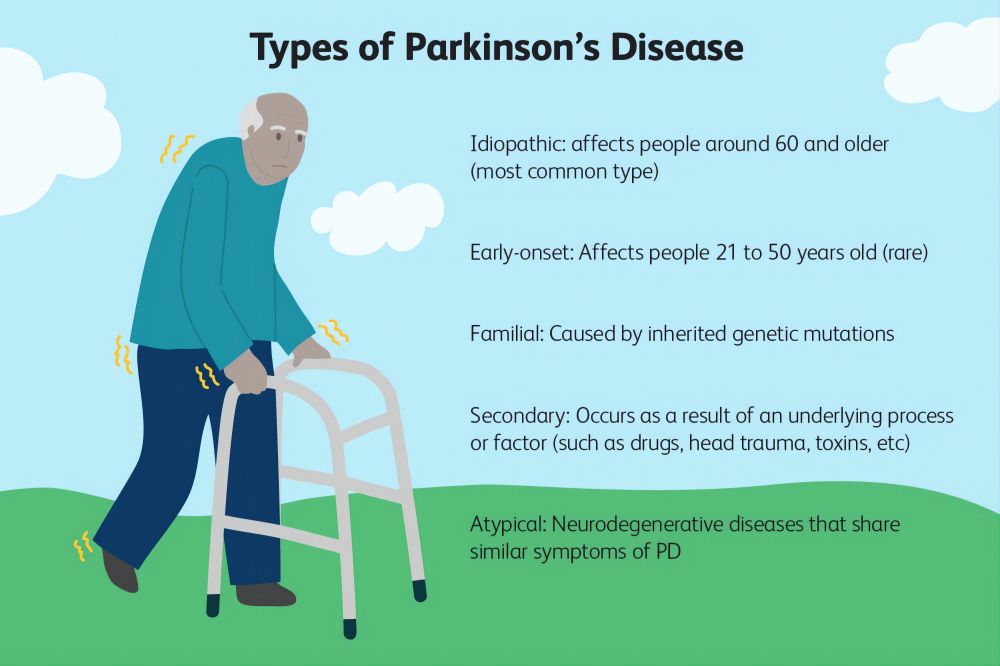
Parkinson's disease, a mysterious and stubborn neurological disease, is known for its gradual attack on the body's ability to control movement. It quietly creeps into the lives of patients, gradually weakening their voluntary movement functions, and eventually affecting all aspects of daily life. However, although Parkinson's disease cannot be cured, the advancement of modern medical technology and assistive devices has given patients more means to cope with the challenges.
In this article, we will explore in detail the definition of Parkinson's disease, its causes, risk factors, symptoms, disease progression, and the medical assistive devices that patients may need.
What is Parkinson's Disease?
Parkinson's disease is a chronic, progressive neurological disease that mainly affects the part of the patient's brain that controls movement. The disease was first described by British physician James Parkinson in 1817, hence the name "Parkinson's disease". The main feature of Parkinson's disease is the gradual loss of dopamine neurons in the substantia nigra region of the central nervous system, resulting in a decrease in dopamine levels. This chemical plays a key role in the brain, helping to coordinate the body's movements. As dopamine decreases, the patient's ability to control movement gradually declines, eventually leading to movement disorders and other non-motor symptoms.
The main symptoms of Parkinson's disease include tremors (common when at rest), muscle stiffness, bradykinesia (movements become slow and difficult), and problems with balance and coordination. These symptoms may be mild at first, but over time, they gradually worsen and eventually seriously affect the patient's daily life and autonomy.
What Causes Parkinson's Disease?
Although scientists have been studying Parkinson's disease for many years, the exact cause of the disease is still not completely clear. Current research shows that Parkinson's disease may be the result of a combination of factors, including genetic factors, environmental factors, and neurophysiological changes.
Genetic factors
A family history of Parkinson's disease may increase the risk of the disease. Studies have found that about 5% to 10% of Parkinson's patients have a clear family genetic background. These inherited forms of Parkinson's disease are often associated with specific gene mutations, such as mutations in genes such as LRRK2, SNCA, PINK1, PARKIN, and DJ-1. However, in most people with Parkinson's, the disease is not inherited, and genes are only one of many risk factors.
Environmental factors
In addition to genetic factors, environmental factors may also play a role in the development of Parkinson's. Exposure to certain harmful substances, such as pesticides, herbicides, and heavy metals, may increase the risk of the disease. Studies have also shown that people living in rural areas or drinking well water may be at higher risk for Parkinson's, although the specific mechanisms of these associations are not yet fully understood. In addition, long-term exposure to industrial chemicals and solvents may also be associated with the development of Parkinson's.
Neurophysiological changes
One of the characteristics of the brain of people with Parkinson's is the loss of dopamine neurons in the substantia nigra region. This change is triggered by a variety of mechanisms, including oxidative stress, mitochondrial dysfunction, protein misfolding, and neuroinflammation. Together, these mechanisms lead to the degeneration and death of neurons, ultimately leading to the symptoms of Parkinson's.
Who is at Risk for Parkinson's?
Parkinson's mainly affects middle-aged and elderly people, especially those over 60 years old. However, this does not mean that young people are completely immune. Early-onset Parkinson's disease, that is, Parkinson's disease patients who develop the disease before the age of 50, also exist in clinical practice.
Age
Age is the main risk factor for Parkinson's disease. As age increases, the risk of Parkinson's disease also increases. Most Parkinson's disease patients develop the disease over the age of 60, which is related to the natural degeneration of the nervous system.
Gender
Studies have shown that men are slightly more likely to develop Parkinson's disease than women. Although the reasons for the gender difference are not completely clear, some studies speculate that it may be related to differences between men and women in nervous system structure, hormone levels, and lifestyle.
Family history
As mentioned earlier, people with a family genetic background have a higher risk of Parkinson's disease. If there is a Parkinson's disease patient in the first-degree relative, the risk of other family members will also increase.
Environmental exposure
Long-term exposure to certain chemicals, heavy metals, and pesticides may increase the risk of Parkinson's disease. Agricultural workers, industrial workers, and people living in rural areas have a higher risk of disease because they have more opportunities to be exposed to these substances.
Lifestyle
Lifestyle factors such as smoking and drinking may also affect the risk of Parkinson's disease. Interestingly, some studies have found that smokers have a lower risk of developing Parkinson's disease than non-smokers, although other health risks from smoking far outweigh this. In addition, the relationship between alcohol consumption and the onset of Parkinson's disease remains uncertain and requires further research.
What are the Early Symptoms of Parkinson's Disease?
An article published by Eric Noyes, MD, of the University of Saskatchewan, mentioned that people with Parkinson's disease experience tremors when their muscles are relaxed, muscle stiffness, slow movements, and problems with balance and walking. The early symptoms of Parkinson's disease may be so mild that they are difficult for the patient or their family to detect. Over time, these symptoms gradually worsen and become more obvious. Knowing the early symptoms is essential for early diagnosis and treatment.
Tremor
Tremor is one of the most common early symptoms of Parkinson's disease and usually starts in the thumb or fingers of one hand. Tremors are usually most noticeable at rest and temporarily relieved when the patient concentrates or exercises. As the disease progresses, tremors may spread to other limbs.
Bradykinesia
Bradykinesia is another early symptom of Parkinson's disease, which manifests as slow and difficult movements. This symptom may make daily activities such as dressing, bathing or eating more strenuous. The patient may feel that the limbs are not as flexible as before, and the gait becomes slow and dragging.
Muscle stiffness
Parkinson's disease patients may have stiff muscles that limit their range of motion. This muscle stiffness affects not only the limbs, but also the muscles in the back, neck, and shoulders. Stiff muscles are often accompanied by pain or discomfort, especially when moving.
Balance and coordination problems
As Parkinson's disease progresses, patients may develop balance and coordination problems, increasing their risk of falling. Early balance problems may manifest as an unstable posture when walking, difficulty turning, or an asymmetrical gait.
Stiff facial expressions
Parkinson's disease patients may lose flexibility in their facial muscles, resulting in a decrease in facial expressions and the so-called "mask face." This symptom makes patients look dull and lack emotional expression.
Micrographia
Parkinson's disease patients may gradually write smaller, irregular, and illegible handwriting. This symptom is called "micrographia" and is one of the manifestations of slow movement.
Other non-motor symptoms
In addition to the above motor symptoms, Parkinson's disease patients may also experience a range of non-motor symptoms, such as loss of smell, constipation, depression, anxiety, sleep disorders, and cognitive impairment. Although these symptoms are less pronounced than motor symptoms, they can also have a profound impact on the patient's quality of life.

Is there a Cure for Parkinson's Disease?
Unfortunately, there is currently no cure for Parkinson's disease. According to the clinical results of a research paper from MovementDisorders: "A total of 59.5% of patients reported a deterioration in their global health status during the COVID-19 emergency. Patients with deterioration did not differ from those referred for stable disease in terms of age, age at onset, sex, and duration of illness. Instead, they had higher scores on PWBM (55.5 ± 30.6 vs. 39.8 ± 32.7; F(1,66) = 7.4, P = 0.008) and BDI (11.3 ± 8.2 vs. 5.9 ± 4.7; F(1,63) = 6.21, P = 0.012), and lower total METs (1714 ± 1570.5 min/week vs. 2399.6 ± 2412.3; F(1,53) = 4.5, P = 0.038). "However, with the advancement of medical technology, the symptoms of Parkinson's disease can still be treated with medication, physical therapy, surgery and lifestyle adjustments, and patients can effectively control symptoms and improve their quality of life.
Medication
Medication is one of the main means of managing Parkinson's disease. The most commonly used drug is Levodopa, which can replenish the lack of dopamine in the brain and relieve symptoms such as tremors, stiffness and bradykinesia. However, long-term use of Levodopa may lead to reduced efficacy and side effects, such as the appearance of motor complications. For this reason, doctors usually combine other drugs such as dopamine agonists, monoamine oxidase inhibitors (MAO-B inhibitors) and anticholinergics to help patients better manage symptoms.
Physical therapy
Physical therapy includes exercise therapy, occupational therapy and speech therapy, which aims to help patients maintain or restore physical function and independence. Exercise therapy helps patients maintain flexibility and mobility by strengthening muscle strength, improving balance and coordination. Occupational therapy focuses on teaching patients how to complete daily activities more effectively, such as dressing, bathing and eating. Speech therapy can help with speech and swallowing difficulties, which are common in people with Parkinson's disease.
How exercise relates to Parkinson's disease:
● Exercise is free, easily accessible, and beneficial for everyone, including people with Parkinson's disease.
● Animal studies suggest that exercise may be neuroprotective and increase the availability of dopamine in the brain.
● There is no clear evidence that exercise can slow the progression of Parkinson's disease, but it has been shown to improve motor symptoms and quality of life.
● The type, intensity, and frequency of exercise may be different for each Parkinson's disease patient, and a personalized exercise plan is recommended.
● Tai Chi, Pilates, and dancing are recommended to help maintain balance and agility.
● Exercising in a group can provide social interaction and fun.
● Walking alone is not enough to challenge the balance system.
● Exercise helps prevent falls and reduce the consequences of Parkinson's disease
Surgery
For patients who do not respond well to medication, surgery may be an option. Deep brain stimulation (DBS) is a common surgical procedure that relieves Parkinson's disease symptoms by implanting electrodes into specific areas of the brain to regulate abnormal brain electrical activity. Although DBS is not a cure for Parkinson's disease, it can significantly improve the quality of life of patients, especially for those who do not respond well to medication.
Lifestyle adjustments
Lifestyle adjustments are essential for symptom management in patients with Parkinson's disease. Maintaining regular exercise and a healthy diet can help enhance the body's adaptability and immune system. Patients should also pay attention to adequate rest and sleep and avoid excessive fatigue. In addition, emotional management and psychological support are also important parts of helping patients cope with the disease.
The relationship between dietary habits and Parkinson's disease:
● A plant-based diet can reduce the risk of Parkinson's disease and control symptoms.
● A diet low in animal fat and high in whole grains and strawberries may effectively reduce Parkinson's disease symptoms.
● Drinking coffee has a protective effect against Parkinson's disease and may slow its progression.
● A six-week study showed that caffeine intake significantly improved Parkinson's symptoms, but this effect tended to weaken with repeated use over time.
● Excessive consumption of soursop (a fruit called graviola) may cause an atypical form of Parkinson's disease.
● High dietary intake of animal fats, iron, mercury, and dairy products may increase the risk of Parkinson's disease.
● Further research is needed to investigate the anti-Parkinson's activity of other edible plants.
How Does Parkinson's Disease Progress Over Time?
Parkinson's disease is a chronic progressive disease, meaning it gradually gets worse over time. Although the rate of progression and the presentation of symptoms vary from person to person, in general, the progression of Parkinson's disease can be divided into five stages.
Stage 1: Early Stages
In the early stages of Parkinson's disease, patients' symptoms are usually mild and may only affect one side of the body. Common symptoms include mild tremors, mild bradykinesia, and muscle stiffness. Patients are usually still able to complete daily activities independently during this stage, and their quality of life remains largely unchanged.
Stage 2: Extended Symptoms
As the disease progresses, symptoms begin to affect both sides of the body. Patients may find themselves unsteady when walking, standing, or turning. Although daily activities can still be completed independently, the worsening of symptoms begins to have a more obvious impact on patients' lives.
Stage 3: Moderate stage
During this stage, the patient's symptoms become more pronounced, and balance problems and risk of falls may occur. Slow movement and muscle stiffness increase, making daily activities more difficult. The patient may need help with some daily tasks, but in most cases, they can still maintain a certain degree of independence.
Stage 4: Severe stage
In stage 4 of Parkinson's disease, the patient's symptoms become very severe. Most patients at this stage require the help of a walker or wheelchair to stay mobile. Daily activities become very difficult, and the patient may need constant nursing support to complete basic tasks.
Stage 5: Advanced stage
The advanced stage of Parkinson's disease is often accompanied by severe movement disorders and cognitive problems. The patient may completely lose independence and require 24/7 nursing support. Some patients may also experience dementia symptoms at this stage, further affecting their quality of life.
What Medical Assistive Devices are Needed for Parkinson's Disease?
7 Types of Medical Assistive Devices Needed for Parkinson's Disease:
1. Walker
2. Wheelchair
3. Lift chair
4. Hospital bed
5. Gait assistive device
6. Swallowing aid
7. Urination and defecation assistive device
As Parkinson's disease progresses, patients may need a variety of medical assistive devices to help them cope with symptoms, maintain independence and improve quality of life. These devices can help patients manage challenges in daily life and reduce the risk of falls and other accidents.

Walker
Walkers are one of the commonly used assistive devices for Parkinson's disease patients, especially when the disease progresses to affect balance and mobility. Walkers provide stable support to help patients maintain balance at home or when going out, reducing the risk of falls. There are many types of walkers, including walkers with wheels and walkers without wheels, and patients can choose the most suitable model according to their needs.
Wheelchair
For Parkinson's disease patients with limited mobility, wheelchairs are indispensable assistive devices. Wheelchairs can help patients maintain mobility at home or when away from home, and reduce the burden on family members or caregivers. The choice of wheelchair depends on the patient's mobility and needs. Electric wheelchairs are suitable for patients with poor mobility, while manual wheelchairs are suitable for patients who need to use it for a short time.
Lift chairs
Lift chairs can help Parkinson's patients move from sitting to standing more easily, especially when muscle stiffness and bradykinesia worsen. This device raises or lowers the seat by an electric device, reducing the patient's effort when getting up and preventing falls.
Hospital beds
Parkinson's disease patients in advanced stages may require the use of specially designed medical beds, which are often adjustable in height, tilt angle, and mattress firmness to provide better comfort and nursing support. Some beds also come with guardrails to prevent falls and controls that are easy for caregivers to operate.
Gait assist devices
Gait assist devices such as gait belts and gait trainers can help patients improve walking posture and gait and reduce the risk of falls. These devices are often used in physical therapy, but patients can also use them at home to help maintain mobility.
Swallowing aids
Parkinson's disease patients may experience difficulty swallowing as the disease progresses, which can lead to malnutrition and the risk of choking. Swallowing aids such as specially designed utensils, cups, and straws can help patients eat and drink more safely.
Urinary and defecation aids
Some Parkinson's patients may experience difficulty urinating and defecating and need to use assistive devices such as catheters, bedpans, or toilets to manage excretion problems. These devices help maintain the comfort and dignity of patients and reduce the burden on caregivers.

What Type of Wheelchair is Needed for Parkinson's Disease?
Types of Wheelchairs Needed for Parkinson's Disease:
1. Manual wheelchair
2. Electric wheelchair
3. Specially designed wheelchair
When choosing a wheelchair, Parkinson's disease patients should consider the patient's mobility, living environment and specific needs. Generally speaking, wheelchairs are divided into two categories: manual wheelchairs and electric wheelchairs. Of course, you can also consider customizing a specially designed wheelchair.
Manual wheelchairs
Manual wheelchairs are suitable for Parkinson's patients who still have some upper limb strength and mobility. Manual wheelchairs are light, easy to operate, and suitable for short-term use or indoor environments. However, for patients with severely limited mobility, manual wheelchairs may not be ideal because they require patients or caregivers to push hard.
Electric wheelchairs
Electric wheelchairs are suitable for Parkinson's patients who have reduced mobility and need more assistance. Electric wheelchairs are battery-powered and equipped with a joystick or control panel, which can be easily controlled by patients and can be moved freely even in confined spaces. Electric wheelchairs are usually equipped with multiple features such as seat tilt, footrest adjustment and head support to provide greater comfort and support.
Specially designed wheelchairs
For some Parkinson's patients with special needs, there are also wheelchairs designed specifically for Parkinson's patients on the market. These wheelchairs may be equipped with anti-tremor devices, special support structures and more stable bases to meet the specific needs of patients.

What Type of Walker Is Needed for Parkinson's Disease?
Types of Walkers Needed for Parkinson's Disease:
2. Wheeled walker
3. Four-wheeled walker
4. Gait trainer
Walkers are an important tool for people with Parkinson's disease to maintain independence. There are many choices of walkers, depending on the patient's needs and the progression of the disease.

Standard walkers
Standard walkers are suitable for patients who are just beginning to need support. This walker is usually wheelless and provides stable support to help patients maintain balance. Standard walkers are suitable for use at home, especially in environments with relatively flat surfaces.
Wheeled Walkers
Wheeled walkers are suitable for patients who need a greater range of motion. The front wheels of this walker can rotate, so that patients do not need to lift the walker when moving, which reduces the burden of use. Wheeled walkers are suitable for use in indoor and outdoor environments, especially when a larger range of motion is required.
Four wheeled walkers
Four wheeled walkers are suitable for Parkinson's patients who need greater support and stability. Four wheeled walkers are usually equipped with hand brakes, seats and storage baskets, so patients can sit and rest when needed, and can carry personal items. Four wheeled walkers are suitable for patients who need to walk for long periods of time or use them when going out.
Gait trainers
Gait trainers are a device designed to improve walking posture and gait. For people with Parkinson's disease, this device can help improve balance and reduce the risk of falls. Gait trainers are often used in physical therapy, but can also be used as daily aids.

Do I Need to Buy a Bed for Parkinson's Disease?
Parkinson's patients may need a specially made bed in the late stages of the disease to provide better comfort and care support. Such beds usually have height adjustment, tilt adjustment, and mattress firmness adjustment functions, which are convenient for patients and caregivers to use. Electric hospital beds are the most common choice for Parkinson's patients. The height, tilt angle, and mattress firmness of such beds can be adjusted by remote control, making it easier for patients to get up, lie down, and turn over. Electric hospital beds are also equipped with guardrails to prevent falls, which helps protect patients' safety.
Secondly, pressure-dispersing mattresses can help prevent pressure sores in Parkinson's patients who are bedridden for a long time. Such mattresses protect patients' skin and tissues by evenly distributing body weight and reducing local pressure accumulation. In addition, bedside rails can help Parkinson's patients get in and out of bed more safely and prevent falls. Lifters can help caregivers take care of patients more easily and reduce physical burden.
In general, although Parkinson's disease cannot be cured, patients can still maintain a certain degree of independence and quality of life through reasonable medication, physical therapy and the use of appropriate medical assistive devices. Understanding the causes, risk factors, and progression of Parkinson's disease and choosing appropriate assistive devices are important steps for patients and their families to meet this challenge.








